The link between stress and depression has been widely investigated throughout scientific research for centuries, where multiple converging factors related to stress have been associated with inducing depressive symptoms and vice versa.

These factors include the dysregulation of the HPA axis, (neuroplasticity) neurotrophic factors, immune system and inflammatory processes.
Role of HPA axis:

The HPA axis has been implicated in the pathophysiology of both stress and depression and functions as the core stress response system. This allostatic, self-regulating process is activated in response to stressors and has also been found to regulate neuroplasticity. HPA axis hyperactivity has been found to be a common neurobiological change in depressed patients where it has been found in 70% of individuals with depression in past research conducted.
The hypothalamic paraventricular nucleus is the main centre located in the hypothalamus. In response to stressors, the HPA axis is activated, releasing corticotrophin-releasing factors (CRF). Research has found an increased CRF immune-reactivity in the Cerebrospinal fluid of individuals with depression (15).
Vasopressin, a neuropeptide that regulates blood pressure and anxiety, is co-expressed via parvocellular neurones, creating a synergistic interaction with CRF.
Studies have shown elevated concentrations of vasopressin in depressed patients, which could potentially contribute to hyperactivity of the HPA axis, whereas selective serotonin reuptake inhibitors (SSRIs) have been found to reverse this.
CRF and Vasopressin stimulate the release of adrenocorticotropic hormone (ACTH), which in turn binds to receptors on the adrenal cortex and increases the release of glucocorticoids; cortisol. Cortisol binds to either mineralocorticoid (MR) in the hypothalamus with high affinity or glucocorticoid receptors (GR) with lower affinity, both of which play a role in negative-feedback mechanisms. Studies suggest the dysregulation of the MR and GR in the HPA axis may lead to depression.
Increased levels of cortisol have been observed in the saliva, blood and urine of individuals with depression along with an increased adrenal gland activity.
Chronic activation of the HPA axis may lead to detrimental effects on the hippocampus, inhibiting neurogenesis.
Long term use of SSRIs and other antidepressants that block 5-HT and norepinephrine uptake has been shown to affect hyperactivity in the HPA axis in depressive patients in a study conducted by Jensen et al. This is supported further by studies that have found that long term treatment via SSRIs normalizes the HPA axis activity. Furthermore, within weeks 2 to 6 of antidepressant treatment, elevated concentrations of MR and GR have been studied, which corresponds to the clinical symptom improvement. This indicates elevated corticosteroid levels contribute to depressed symptoms.
Role of immune system and inflammatory responses:

The effects of the immune system and inflammatory responses on depression and psychological stress has been researched in over the last several decades.
Chronic stress has been demonstrated to activate inflammatory responses through the activation of the sympathetic branch of the autonomic nervous system, which increases pro-inflammatory cytokines of the immune system such as such as tumour necrosis factor-alpha (TNF-α) and interleukin-1β. These cytokines have also been found to be elevated in depressed individuals indicating a link between stress, depressive symptoms and the immune system. This as excessive release of pro-inflammatory cytokines can lead to a decreased level of BDNFs and neurogenesis along with impaired neuroplasticity, factors of which have been associated with the origin of cognitive impairment and mood disorders.
Cytokines have also displayed the ability to increase monoamine re-uptake, thus reducing the concentrations of neurotransmitters in the brain and are thought to contribute to depressive symptoms such as cognitive dysfunction and insomnia.
The cytokine protein interleukin-1β beta is located primarily in the hypothalamus and is expressed through interacting with the interleukin-1R1 receptor. Chronic exposure to stress increases the release of the interleukin-1β in the hypothalamus, consequently inducing the activation of HPA axis and a decreased expression of BDNF. This cytokine is also linked with the regulation of the serotonin transporter gene, an important factor in SSRI antidepressants, suggesting a link between the immune system and depressive symptoms.
Although interleukin-1β plays a vital role in the modifying of neurotransmitters, other factors such as TNF-α, IL-2 and IL-6 also contribute to a lesser extent. Stress could potentially lead to serotonergic neurotransmission dysregulation which in turn could play a role in depressive symptoms. This is supported by a study conducted by Kraus et al, where healthy participants given low dosages of endotoxin, which increased the IL-6 and TNF-α concentrations positively correlated with depressive moods, anxiety and memory impairments. However, a correlation does not imply causation and therefore further research should be conducted to provide with a depth understanding.
Furthermore, TNF-α, a multifunctional signaling molecule, is involved in activation of the HPA axis, leading to the release of CRFs, which may lead to hypercortisolism. This results in decreased activity of tryptophan hydroxylase and consequently a lower 5-HT synthesis. The activation of the HPA axis also stimulates the enzyme, indoleamine-2,3-dioxygenase. This catabolizes the α-amino acid, tryptophan through the kynurenine pathway, leading to decreased 5-HT synthesis and secretion. 3-hydroxykynurenine is produced through the catabolism of kynurenine resulting in the activation of the glutamatergic system through kynurenic acid and free radicals, this is an area researchers have linked to the pathogenesis of depression.
TNF-α has serotonin reducing effects which indicates that inhibiting the signaling of TNF-α may alleviate depressive symptoms. This has the same effect as SSRIs, where serotonin re-uptake is blocked. This is further supported by research findings where deletion of the TNF-αR1 gene has led to decreased depressive symptoms in mice.
A more in depth understanding of the impact of pro-inflammatory cytokines responses in association to depressive symptoms has enabled studies aimed at finding treatment in relation to these processes to be conducted allowing studies to establish the efficacy of these cytokines in inhibiting depressive symptoms using in vivo procedures.
Diseases such as arthritis that initiate inflammatory responses have been linked to depression, where it is apparent that inflammation causes depression and the vice versa effect with depressed patients is possible. This can be linked to stress as studies have concluded that depressive patients had enhanced inflammatory response to psychological stress compared to those without depression, thus suggesting increased vulnerability. This can be supported by research that found depressed patients exhibited enhanced inflammatory responsiveness to mild psychosocial stress caused by public speaking through an increased IL-6 and NF-kappaB activity.
Neuroplasticity:
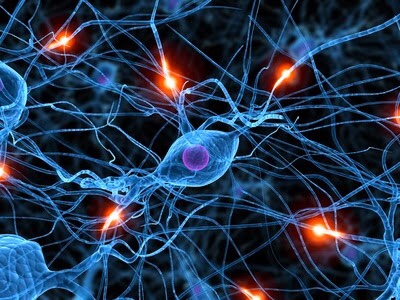
Neuroplasticity plays a vital role in the pathology of depression by affecting the regulation of neurogenesis, along with synaptic plasticity. Neurotrophic factors such as BDNF effect the neuronal plasticity and functioning of the brain along with the nervous system. The role of brain-derived neurotrophic factor (BDNF) has been assessed thoroughly, where lower BDNF levels in blood cells of depressed patients. Furthermore, abnormalities in BDNF functioning due to impaired receptors in the brain of depressed subjects. BDNF has been suggested to decrease 5-HT uptake in vitro testing. Overall, BDNF has shown to be implicated in the pathogenic mechanisms of depression. Further studies are required to describe how BDNF is involved in these depressive symptoms.
There have also been strong links between stress and BDNF found in the brain. Exposure to stressors may lead to decreased hippocampal neurogenesis and BDNF expression. A study conducted by Makino et al indicated that chronic immobilization stress lead to decreased mRNA expression of BDNF in the brain. Furthermore, the role of BDNF on stress studied in rodents by exposure to corticosterone has also been found to decrease the BDNF expression in the brain (39). This was further supported as it was observed that the mRNA level of BDNF decreased in the hippocampus and frontal cortex when exposed to corticosterone, whereas the withdrawal of corticosterone lead to an increase BDNF level in the hippocampus. These studies have consistently demonstrated a decreased BDNF levels caused by stress that, however, could be reversed by antidepressant treatment.
Antidepressant drugs such as SSRI have also been demonstrated to increased BDNF expression in the cortical regions and hippocampus of the brain. To have a more in-depth understanding of the role of BDNF in antidepressants, a small dosage of BDNF protein was infused directly into the CA3 and DG region of the brain and concluded that this was sufficient enough to cause antidepressant-like response within 3 days, emphasising the importance of these regions for BDNF having antidepressant effects. Furthermore, a decrease in BDNF in the DG region was found to be vital for the antidepressant-like responses of conventional antidepressants such as SSRIs, suggesting BDNF in the DG region of the hippocampus is needed for antidepressant efficacy.
BDNF has also demonstrated antidepressant-like properties in rodents and can block antidepressant effects of drugs such as SSRIs via genetic deletion thus could potentially new render therapeutic targets. However, studies on rodents have found insufficient evidence for BDNF causing depression and thus argues that it is only an alternative component factor that potentially leads to depression.
Furthermore, the changes in pro-inflammatory cytokines due to prolonged activation of the inflammatory processes in the brain compromises cognitive function and neuroplasticity. This induces decreased neurogenesis, neurotrophins and neuron repair along with enhanced oxidative stress and neuron apoptosis.
Role of serotonin and vasopressin:

Serotonin and its receptors are a key target for SSRI drugs to alleviate depressive symptoms and contribute to symptoms of depression such as anxiety, pessimistic moods and sleep disturbance. Increased stress levels can also be linked to serotonin as the serotonergic system is closely linked to cortisol concentration. The 5HT 1A receptors are highly expressed on serotonergic neurons and located in the hippocampus playing a key role in stress anxiety and depression. Studies have correlated a decrease in 5HT1A receptors activity with increased stress levels. Mineralocorticoid receptors impact the 5HT1A receptor cells as their activity decreases under stressful conditions. In contrast to this, the auto receptors 5HT1B and are activated by stress. This could be used to explain reduced serotonergic activity in depressed patients through glucocorticoids caused by stressors.
Serotonin is a monoamine transmitter synthesized from tryptophan. Recent findings suggest that impaired functioning of serotonin could lead to depression through tryptophan. This is as changes in tryptophan concentrations have been found to lead to corresponding changes in the ability for neurons to produce 5-HT. The essential amino acid, tryptophan hydroxylase has been reported to have significantly lower concentrations in depressed individuals. Furthermore, this is also supported by research conducted where acute dietary manipulation where low-tryptophan supplemented with high neutral amino acid dosage lead to the depletion of tryptophan in depressed individuals. The neutral amino acids are thought to have increased the reduction of the serotonin in the brain via tryptophan depletion as it was used as competition with tryptophan for carrier-mediated brain uptake. It was found that this diet lead to the relapsing of depressed individuals taking antidepressant drugs such as fluoxetine and desipramine within several hours of indigestion. Moreover, these individuals were found to have improvements in depressive symptoms when provided by tryptophan supplements suggesting that alterations in the serotonin concentration in the brain has a significant impact on the intensity of the symptoms experienced by depressed patients and that robustness of the serotonergic neuronal activity is vital for the therapeutic response of specific antidepressants.
Furthermore, the Antidiuretic hormone, vasopressin impacts the HPA axis through binding to the V1b receptors located in the brain. Research over the years have consistently found elevated levels of vasopressin in depressed patients along with a hyperactive HPA axis. It has been found that depressed individuals have a higher number of V1b receptors compared to individuals that do not have depression. This suggests a link between vasopressin, the HPA axis and depression

 Microbes, collectively, include bacteria, viruses, fungi, and parasites. Antimicrobial drugs, such as antibiotics, have been successfully used to treat patients with bacterial and infectious diseases. Antibiotics may either kill or inhibit the growth of bacteria. Antibiotics are not effective against viruses such as the common cold or influenza.
Microbes, collectively, include bacteria, viruses, fungi, and parasites. Antimicrobial drugs, such as antibiotics, have been successfully used to treat patients with bacterial and infectious diseases. Antibiotics may either kill or inhibit the growth of bacteria. Antibiotics are not effective against viruses such as the common cold or influenza.